Bones & Muscles
Musculoskeletal issues
Our bones, cartilage, muscles, joints, tendons and ligaments are all part of our musculoskeletal system. Musculoskeletal issues are quite common in people who have Down’s syndrome. There are different reasons for this including low muscle tone, lax ligaments and hypermobile joints.
There is further information about the more common musculoskeletal issues seen in people who have Down’s syndrome in our resource ‘Orthopaedic issues’ which is linked to below. Orthopaedics is the branch of medicine that deals with issues involving the musculoskeletal system. Neck instability is covered in a separate resource.

Neck Instability
Underlying neck instability is more common in people who have Down’s syndrome than in the general population. This causes concern because although significant damage caused by neck instability is rare and most people have mild early warning signs, it can be devastating and result in paralysis and in extreme cases death.
Parents, carers and practitioners should be constantly aware of the warning signs (symptoms) which might indicate that a person who has Down’s syndrome is at risk of neck instability. If parents, carers or people who have Down’s syndrome suspect any of the signs or symptoms listed here (a), (b), the person may have a problem with neck instability and should be seen by a Doctor.
A) Warning symptoms:
- Pain anywhere along the neck
- A stiff neck which doesn’t get better quickly
- Unusual head posture (‘wry neck’ or torticollis)
- Alteration in the way a person walks so they may appear unsteady
- Deterioration in a person’s ability to manipulate things with his/her hands.
B) Poor neck control:
- Difficulty holding the head up
- Holding the head at an unusual angle
- Difficulty nodding or looking up and down and/or difficulty turning the head in certain directions.
Further Information on Neck Instability
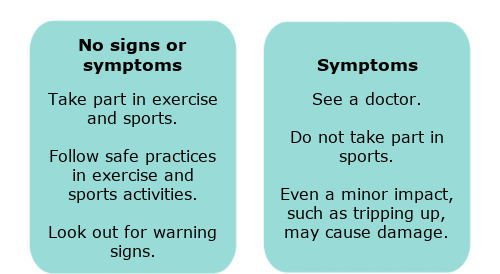
Anyone with the above signs could have underlying neck instability and be at increased risk of neck dislocation. Minor impact involving the person with the symptoms may cause spinal damage (e.g. tripping up or a jolt). Any parent, carer or sports coach with concerns about a person’s neck control or any emerging warning signs before, during or after sport sessions, must refer the person for medical assessment.
Neck instability is a highly specialised area of medical practice. The Doctor may refer the person to a specialist centre. For people who have Down’s syndrome who have no symptoms (the majority), there are no reliable tests that can identify those at increased risk of neck instability.
Safe sporting practices, such as appropriate supervision, are essential.
For people who do not have symptoms of neck instability, there should be no additional anxiety about them taking part in non-contact, low impact sporting activities. Some sports such as trampolining, diving, contact sports and high jump have higher risk for neck injury in all participants (people who do not have Down’s syndrome as well as people who do).
Ask the sports provider or National Governing Body of the sport about their safe sporting practices and eligibility criteria. Based on current information, it is sensible advice for adults who have Down’s syndrome to travel in cars with headrests and for children to travel in car seats with neck support.
People who have Down’s syndrome who are unconscious are potentially at risk for neck damage. Ambulance personnel and healthcare professionals, including anaesthetists, know how to take special care of the neck in these circumstances.
Any signs, symptoms or loss of skills?
There is more in-depth information about neck instability in our resources section at the bottom of the page.
Arthritis And Osteoporosis
Arthritis And Osteoporosis In Adults
Osteoporosis affects the bones; as we get older our bones become thinner, more porous and therefore weaker. The bones are therefore more susceptible to fracture. Amongst other things the condition is associated with increasing age and a decrease in oestrogen after the menopause in women. Men in the general population are susceptible to osteoporosis but not as much as women are.
There is some evidence to suggest that both men and women who have Down’s syndrome may be more at risk of osteoporosis. A healthy calcium rich diet, vitamin D and regular exercise can help to improve bone density and thus reduce the chance of developing osteoporosis. Often there are no symptoms but sometimes there may be a change in the way a person walks. If osteoporosis is suspected, a bone density test may be carried out.
Rheumatoid arthritis is an autoimmune condition which results in inflammation in the joints. It is more commonly seen in the hands, wrist, ankles and foot bones but it can affect any joint. Osteoarthritis affects mainly the large joints (e.g. back, shoulders, knees, hips) and it occurs because of wear and tear on the joints. It results in inflammation and degeneration of the joints.
Some adults who have Down’s syndrome may develop osteoporosis and arthritis at an earlier age than is seen in the general population. This may be because of lower levels of exercise and the early onset of menopause amongst other things.
Arthritis In Children
Arthritis (inflammation of the joints) is an autoimmune condition. Children who have Down’s syndrome have an increased risk of autoimmune conditions. Autoimmune conditions are caused by a malfunction in the body’s natural defence systems against infections. The small but slowly growing body of evidence suggests there is an increased risk of an inflammatory form of arthritis in children who have Down’s syndrome.
Health professionals call this condition ‘Inflammatory arthritis of Down’s syndrome’ (our preferred term). However, you may hear some health professionals refer to this condition as ‘Down’s arthropathy’.
Inflammatory arthritis of Down’s syndrome is an under-recognised condition that, if untreated, results in chronic disability and functional impairment. Greater awareness of the increased risk of this condition will lead to earlier diagnosis and treatment.
Children who have Down syndrome may not easily express the pain that they are experiencing. A change in your child’s ability to perform daily living activities, e.g. in their handwriting or walking abilities may be an indication of early onset arthritis. Seek advice from your doctor if your child is experiencing any of these difficulties or if you are concerned.
There is further inform ation about this condition in our resource ‘Inflammatory arthritis in children’ linked in the resources section.
Further Info & Advice
If you have any questions about health issues, you can call DSA’s Helpline (Tel: 0333 1212 300) or email using info@downs-syndrome.org.uk. If an information officer is unable to answer your question, they can make a referral to the medical adviser at the UK & Ireland Down Syndrome Medical Interest Group (DSMIG).
Please note DSMIG can provide general advice about health issues but they are not able to comment on individual test results. DSMIG are happy to take enquiries from health professionals but they will not take direct from enquiries from families or supporters.